Wound care | Te maimoatanga ō ngā taotū (Frailty care guides 2023)
To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Treatment
- Further resources
- Decision support
- Dressing product types
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
Wound care is the practice of providing the optimum environment for a wound to progress towards healing. Wound healing is a staged process, and wound care goals should match the medical needs of the patient, the stage of wound healing and the patient’s individual goals. Wound care goals help with selecting the appropriate wound dressing.
Key point
- You must conduct a wound assessment before setting wound care goals.
Why this is important
Wounds have significant implications in terms of quality of life and financial burden.
Implications for kaumātua*
Māori have a holistic view of health and wellbeing. It is important to treat the ‘whole person’ and not just ‘the hole in the person’. Taking a holistic approach is one way of protecting the mana (inherent dignity, prestige, status) of kaumātua.
Traditionally, mana increases with age (so kaumātua are highly regarded), and as mana increases so does tapu (sacredness) (Mead 2016). All people (and their body fluids) are tapu (sacred, prohibited, restricted); the head and sex organs are the most tapu of all. Items that touch the body and especially the head carry the individual’s tapu.
It is vital to keep tapu and noa (neutral, ordinary, unrestricted) separated from each other and balanced to avoid a breach of tapu. Traditionally, breaching tapu brings on the wrath of the atua (gods), which can have significant spiritual and emotional impact on kaumātua and whānau/family.
Practically this means:
- avoiding damage to tapu and mana by asking for permission to enter personal space (tapu) and to touch the person; touching the head in particular is seen as an intimate act
-
separating tapu and noa by keeping wound care items off food or drink surfaces, away from toileting equipment and away from the head and the pillows that the head rests on.
A wound, particularly one that is large, easily visible or malodourous, may be a source of whakamā (shame, embarrassment) for kaumātua. Kaumātua may find it difficult to show the wound to an outsider or may not want to burden others. As a result, they may be reluctant to have wound care or may inaccurately report their wound issues.
Kaumātua and whānau/family may have culturally informed interventions that support wound treatment from a holistic perspective, including the use of rongoā Māori (traditional Māori medicines) and in some cases pure (cleansing rituals). Explore these options on a case-by-case basis.
See the Guide for health professionals caring for kaumātua | Kupu arataki mō te manaaki kaumātua for more information.
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Assessment
The ideal dressing should: (Turner 1979, WUWHS 2019)
- maintain an optimal moist environment
- remove excess exudate
- allow gaseous exchange
- thermally insulate
- be impermeable to micro-organisms
- be free from contaminants
- be able to be removed without causing trauma.
Take account of factors specific to the patient, including:
- allergies or skin sensitivities
- comfort and conformability
- ease of use
- mana and whakamā
- cost effectiveness
- wound care goals.
Infection control with dressing products
- Store dressing in original containers in a store cupboard (not on treatment trolley).
- Check expiry dates of dressings before using.
- Clean dressing/procedure trolley before and after use.
- Use dressing of the correct size where possible so you do not need to cut sterile dressings.
- If you need to cut dressings, use sterile scissors and throw away any unused product.
Treatment
Wound cleaning
Cleaning wounds with tap water does not increase or decrease risk of infection. Cleaning should focus on removing products that delay wound healing (Fernandez and Griffiths 2012, IWII 2022). The following are suggested cleaning processes.
- Acute wounds (eg, new skin tear): Clean with warm, sterile normal saline.
- Established or chronic wounds: Clean with warm tap water (previously boiled or town supply) or chronic wound cleansers.
- Showering with chronic wounds: Remove dressings in shower to clean chronic wounds.
- Granulation tissue: Clean only if there is a build-up of exudate.
- Sloughy/necrotic tissue: Remove loose slough (gentle irrigation or swabbing), tough stuck necrotic tissue or slough. Consider debridement.
Wound debridement
Autolytic debridement (where the body naturally breaks down dead tissue) is the main method for non-specialists to undertake debridement. The most common approach is to use moisture-retentive (hydrofibre or foam) or moisture-donating (hydrogel or hydrocolloid) dressings.
If sharp debridement is necessary, a health professional with appropriate skills must undertake it. Generally, you will need to make a referral to a wound specialist, general practitioner (GP) or nurse practitioner (NP) (Phillips et al 2020).
Avoid moist wound healing on necrotic tissue or ischaemic wounds until a GP or NP has reviewed the wound. Consider a specialist review.
Choosing a wound dressing
Use a systematic process to evaluate each aspect of the wound – see the decision-support flowchart on the next page.
Match your choice of dressing products to the person’s wound care goals. This guide does not recommend a specific manufacturer. Please refer to the manufacturer information for details on the specific dressing you choose.
Further resources
Carville K. 2012. Wound Care Manual (6th ed, revised and expanded). Perth: Silver Chain Foundation.
Decision support (Leaper 2012, IWII 2022)
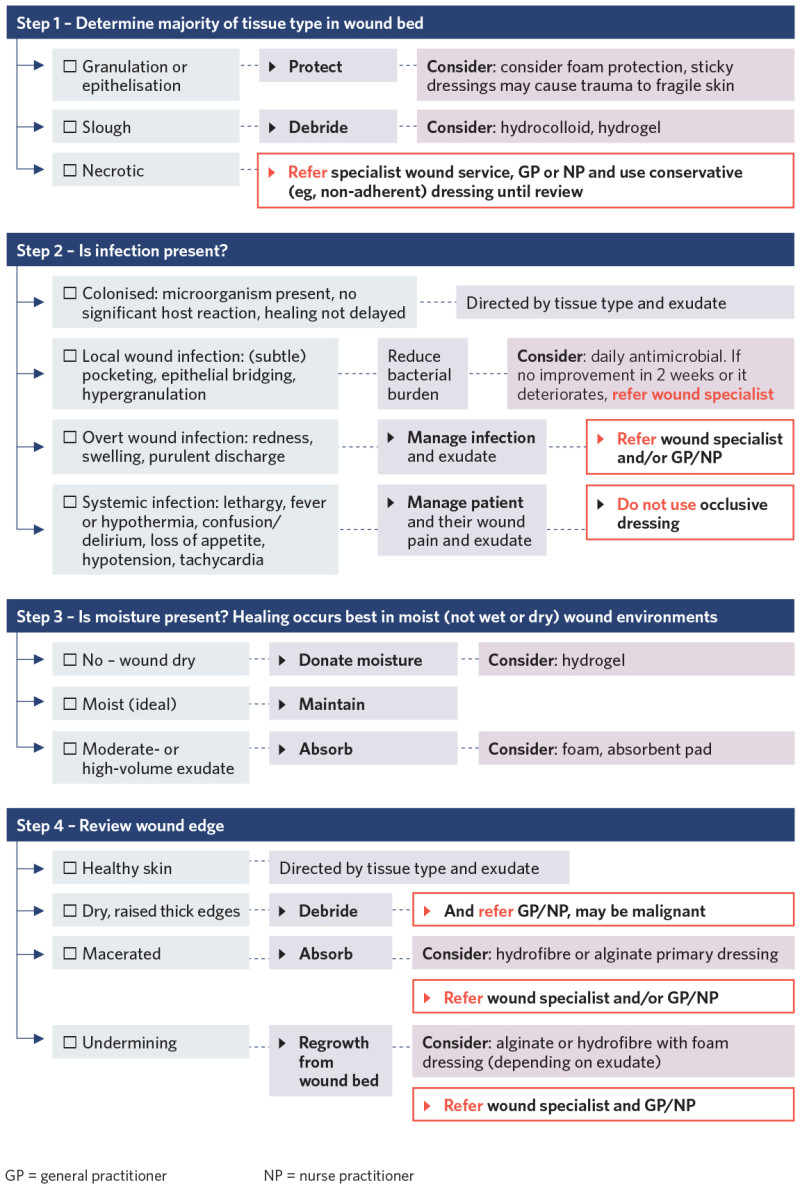
View a higher resolution version of this image in the relevant guide.
Dressing product types
Hydrogel: an aqueous gel with high water content and polymers that absorb some fluid
Indicated for: Dry wounds or hydration of necrotic or sloughy tissue or preservation of bone or tendon
Advantages
- Donates moisture to wound for debridement
- Absorbs some exudate (minimal)
- Easily irrigated from the wound
Care required
- Need to manage surrounding skin to prevent maceration
Practice tips
- Secondary dressing: Use semi-permeable film for dry wounds and a film-coated dressing for low-exuding wounds
Hydrofibre
Indicated for: Wounds with moderate to heavy exudate, or superficial or cavity wounds, or sloughy or granulating wounds
Advantages
- Does not need to be cut to size of wound
- Highly absorbent
- Forms a cohesive gel
- Helps with autolytic debridement
Care required
- Requires a secondary dressing such as an absorbent pad or foam dressing
- Needs sufficient exudate to form a gel
- Dressing expands with absorption of exudate
Practice tips
- Do not moisten before applying to wound
- Has a wear time of up to 7 days
- Seek advice before inserting dressings into cavities where you cannot see the base of the wound
- Cavity wounds: Use rope and fill to three-quarters of wound space – do not overpack
- Deep cavity wounds: Leave a long wick protruding from wound
Alginate: Non-woven fibres of sodium and calcium salts of alginic acid, derived from seaweed
Indicated for: Managing bleeding wounds or wounds with moderate to heavy exudate
Advantages
- Highly absorbent
- Helps with haemostasis
- Helps with autolytic debridement
Care required
- Requires a secondary dressing
- Needs sufficient exudate to form a gel
- Needs to be cut to size of wound
Practice tips
- Do not moisten before applying to wound
- Has a wear time of up to 7 days
- Seek advice before inserting dressings into cavities where you cannot see the base of the wound
Foam: An absorbent multi-layer dressing that maintains an optimal moist environment
Indicated for: Wounds with moderate to heavy exudate or hypergranulating wounds, or cavity or superficial wounds, or sloughy or granulating wounds
Advantages
- Highly absorbent
- Thermally insulating
- Permeable to gas and water vapour
- Impermeable to micro-organisms
- Retains absorbency under compression
- Highly conformable
- Silicone options available for fragile skin
Care required
- Not suitable for dry wounds
Practice tips
- Extend dressing 2 cm beyond wound margins
- Use only non-adhesive foam tape edges (to maintain vapour transmission)
- Has a wear time of up to 7 days
- Check manufacturer instructions for which side to place against wound
Silicone wound contact layer dressing (Meuleneire and Rücknagel 2013): Soft, tacky dressings that do not stick like a traditional adhesive so are less likely to harm fragile skin when you remove them
Indicated for: Skin tears or skin abrasions/lacerations, or surgical wounds, or leg and pressure ulcers
Advantages
- Does not adhere to wound bed
- Minimises pain and trauma during dressing changes
- Comfortable
- Leaves no residue
- Allows passage of exudate
Care required
- Needs secondary dressing to manage exudate
- Do not use if patient has silicone allergy
Practice tips
- Use with secondary dressing
- Can remain in place for up to 2 weeks (depending on wound)
Antimicrobial dressing (Shultz et al 2015; Swanson et al 2022): Reduces bacterial burden and aids healing in critically colonised wounds; its most common additives are iodine silver and honey
Indicated for: Critically colonised wounds
Advantages
- Reduces bacterial burden
Care required
- Not indicated when there is no evidence of critical colonisation
- Patients can be sensitive or allergic to the additive
Practice tips
- Refer to manufacturer’s instruction
References | Ngā tohutoro
Fernandez R, Griffiths R. Water for wound cleansing. Cochrane Database Syst Rev 2012, Issue 2, Art. No.: CD003861. DOI: 10.1002/14651858.CD003861.pub3.
International Wound Infection Institute (IWII). 2022. Wound Infection in Clinical Practice. London: Wounds International. URL: woundsinternational.com/wp-content/uploads/ sites/8/2023/05/IWII-CD-2022-web.pdf.
Leaper D, Shultz G, Carville K, et al. 2012. Extending the TIME concept: what have we learned in the past 10 years? International Wound Journal 9 (Suppl. 2): 1–19. URL: www.cdhb.health.nz/Hospitals-Services/ Health-Professionals/Education-and-Development/Study-Days-and-Workshops/Documents/ Extending%20TIME.pdf.
Mead HM. 2016. Tikanga Māori: Living by Māori values. Wellington: Huia Publishers.
Meuleneire F, Rücknagel H. 2013. Soft silicones made easy. Wounds International May. URL: www.woundsinternational.com/resources/details/soft-silicones-made-easy.
Phillips J, Gruys C, Dagger G. 2020. Advisory Document for Wound Bed Preparation in New Zealand: Advancing practice and knowledge in wound management. New Zealand Wound Care Society. URL: www.nzwcs.org.nz/images/publications/Wound_Bed_Preparation_June2020/ NZWCSWoundBedPrepAdvisoryDoc2020.pdf.
Shultz G, Swanson T, Grothier L. 2015. Wound infection made easy. Wounds International February. URL: www.woundsinternational.com/resources/details/wound-infection-made-easy.
Swanson T, Ousey K, Haesler E. 2022. Wound infection in clinical practice: principles of best practice. Wounds International March. URL: www.woundsinternational.com/resources/details/wound-infection- in-clinical-practice-principles-of-best-practice.
Turner T. 1979. Hospital usage of absorbent dressings. Pharmaceutical Journal 222: 421–6.
World Union of Wound Healing Societies (WUWHS). 2019. Consensus Document. Wound exudate: effective assessment and management. London: Wounds International. URL: woundsinternational. com/wp-content/uploads/sites/8/2023/02/836aed9753c3d8e3d8694bcaee336395.pdf.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
