To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Treatment
- Care planning
- Decision support
- Further resources
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
A pressure injury is localised damage to skin and underlying tissue that occurs as a result of pressure, friction or shearing forces. It can develop when pressure temporarily cuts off circulation and tissue dies. Most pressure injuries develop over bony prominences, especially the sacrum, hips and heels, but they can occur in other areas (EPUAP/NPIAP/ PPPIA 2019).
Why this is important
Pressure injuries are considered avoidable and have a significant impact on quality of life.
Implications for kaumātua*
It is important to give kaumātua and their whānau/family all the information they need to participate in pressure injury prevention and treatment. If they have a strong sense of pride or do not want to be a bother, kaumātua are less likely to ask for or accept help with pressure injury prevention. Whānau/family can suggest valuable, culturally informed interventions and help motivate kaumātua because they are invested in the outcome for their loved one.
Be aware of the concepts of tapu (sacred, prohibited, restricted) and noa (neutral, ordinary, unrestricted) if using pillows for positioning or pressure avoidance. People and their bodily fluids are considered tapu, and items that touch the body, particularly the head, carry tapu from the individual. Do not swap pillows and pillowcases that have been supporting the head with pillows that have been supporting other parts of the body. Doing so would be a breach of tapu and can have a significant negative impact on kaumātua and whānau/family spiritually and emotionally. See the Guide for health professionals caring for kaumātua | Kupu arataki mō te manaaki kaumātua for more information).
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Assessment
- Assess all residents for risk of developing pressure injuries, using a standard risk assessment tool (see the policy of your own facility for the tool of choice). Tools differ in their diagnostic accuracy (Chou et al 2013).
- Implement a pressure injury prevention plan for every resident who is considered at risk of pressure injury.
-
If a pressure injury develops, base wound care on wound assessment and the wound care goal (see the guides to Wound assessment | Te aromatawai taotū and Wound care | Te maimoatanga ō ngā taotū). Reducing pressure, friction or shearing forces is the key to healing.
Treatment
- Report pressure injuries in line with your facility’s policy.
- To stage pressure injury, follow an agreed standard (European Pressure Ulcer Advisory Panel et al 2019) recommended by the Pan Pacific Pressure Injury Classification system (pictures on following pages) and use further resources pppia.org/pppia-resources.
- Pressure injuries in darker skin tones may be more difficult to identify, and this may lead to identification at a later stage (Oozageer Gunowa et al 2018). Specifically, stage 1 pressure injuries are unlikely to be reddened; however damaged skin is likely to be different from surrounding skin in that it may be a different colour, firmer, softer, warmer or cooler than surrounding tissue. The area is also likely to be painful (Baker 2016).
- Use pressure-relieving equipment and techniques in line with your facility’s policy.
- Chart and evaluate progress of the wound every 2 weeks.
- Treat the wound based on the wound care goal.
- Provide adequate pain management, nutrition and hydration. Manage continence and provide associated skin care (see the SSKIN poster).
- Refer high-risk wounds (stage 3 and above) to a specialist wound service and the responsible general practitioner or nurse practitioner.
Care planning
The care plan includes specific pressure areas of care and holistic frailty management, with the aim of maximising wellness and minimising the risk of developing further pressure injuries.
Pan pacific pressure injury classification system for older adults
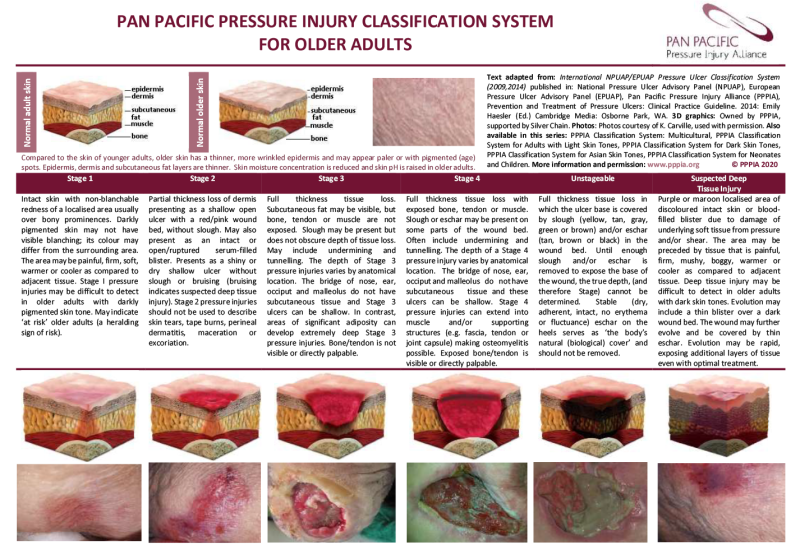
View a higher resolution version of this image in the relevant guide.
Pan pacific pressure injury classification system for dark skin tones
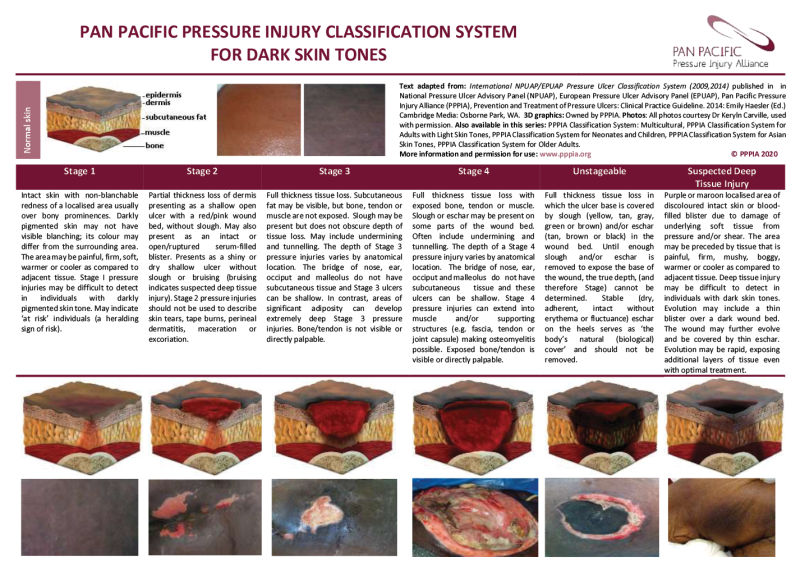
View a higher resolution version of this image in the relevant guide.
Decision support
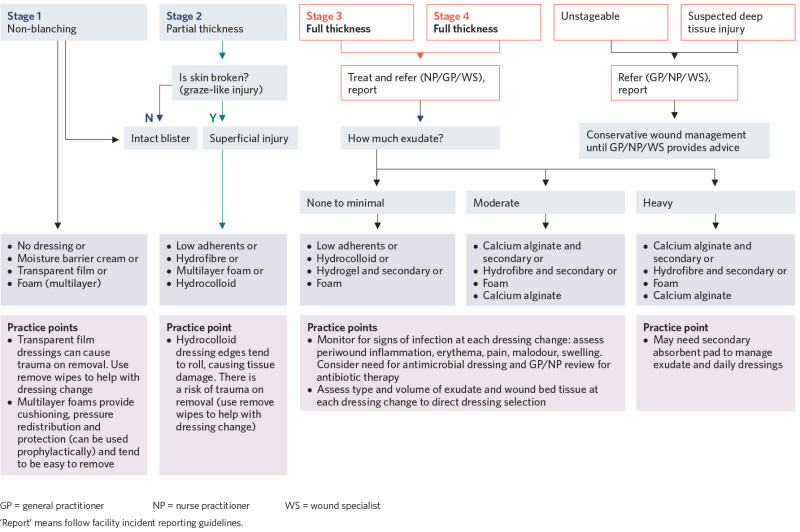
View a higher resolution version of this image in the relevant guide.
Further resources
Pan Pacific Pressure Injury Alliance (PPPIA) resources: pppia.org/pppia-resources
Reproduction of the PPPIA classification system tools and flowcharts is permitted for all educational purposes in the original formats (including acknowledgements and logos) available on the above website.
Advisory Document for Wound Bed Preparation in New Zealand: nzwcs.org.nz/images/publications/Wound_Bed_Preparation_June2020/NZWCSWoundBedPrepAdvisoryDoc2020.pdf
SSKIN (Surface, Skin, Keep moving, Incontinence, Nutrition) poster: www.nzwcs.org.nz/images/ppig/STOP_PI_2020_RESOURCES/3054_ACC_Pressure_Injuries_-_A3_ Poster_FA_ONLINE_PRINT_SSKIN.pdf.
References | Ngā tohutoro
Baker M. 2016. Detecting pressure damage in people with darkly pigmented skin. Wound Essentials 11(1): 28–31. URL: www.wounds-uk.com/resources/details/wound-essentials-11-1-detecting-pressure- damage-in-people-with-darkly-pigmented-skin.
Chou R, Dana T, Bougatsos C, et al. 2013. Pressure ulcer risk assessment and prevention: a systematic comparative effectiveness review. Annals of Internal Medicine. DOI: 10.7326/0003-4819-159-1-201307020-00006.
European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance (EPUAP/NPIAP/PPPIA). 2019. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical practice guideline. The International Guideline. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. URL: internationalguideline.com/2019.
Oozageer Gunowa N, Hutchinson M, Brooke J, et al. 2018. Pressure injuries in people with darker skin tones: a literature review. Journal of Clinical Nursing 27: 3266–75. DOI: 10.1111/jocn.14062.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
