Nutrition and hydration | Te taiora me te mitiwai (Frailty care guides 2023)
To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Care planning
- Nomogram
- Decision support
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
Eating and drinking are fundamental to life. To maintain health, people need to consume a diet that meets the energy and nutrient needs of the body. Human bodies are about 55 percent water, and normal bodily functions rely on adequate hydration (Popkin et al 2010).
Key points
- Age-related changes, cognitive decline and frailty combine to increase the risk of malnutrition and dehydration in older people (Hooper et al 2016; Lukito 2021).
- Cognitive, bladder and bowel function are sensitive to nutrition and hydration status.
- Both food and fluids provide nutrition and hydration. Total water intake includes food sources such as fruit and vegetables (Masot et al 2020), while some liquids such as soups and supplements provide nutritional value.
Why this is important
For people living in aged residential care (ARC), dehydration increases the risk of mortality and rates of delirium and is associated with reduced cognitive function and speech difficulties (Hart et al 2020). In addition, a lack of dietary protein can contribute to sarcopenia (loss of skeletal muscle and strength), which is associated with a loss of function and is a key marker of worsening frailty.
Implications for kaumātua*
Consider three key interacting Māori cultural beliefs when supporting kaumātua with eating and drinking:
- mana (dignity, prestige, status) – kaumātua have a lot of mana, which increases as they age
- tapu (sacred, prohibited, restricted) – as mana increases, so does tapu (Mead 2016)
- noa (neutral, ordinary, unrestricted).
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Eating and drinking
Kai (food) is very important in Māori culture; it is believed to originate from the atua (gods).
- Kai nourishes the tinana (the body), hinengaro (mind), wairua (spirit) and whānau/family (community).
- Kai is a key way of demonstrating manaakitanga (hospitality, caring for others).
- People share kai as part of whanaungatanga (connecting) and belonging to a collective.
-
Specific tikanga (customary practices or behaviours) are associated with kai.
Tikanga around kai
Maintaining a separation and balance between tapu and noa is vital. When this is not maintained, a breach of tapu occurs, and traditionally this is thought to incur the wrath of the atua (gods). A breach of tapu can be significant for kaumātua and their whānau/family.
Kai and wai (water) are considered noa, while people and their bodily fluids are considered tapu. Items that touch the body, particularly the head (eg, hairbrush, toothbrush, clothing, bedding) carry tapu from the individual. This tapu can be neutralised, but until that happens, such items should be kept away from food.
The following guidelines can help maintain balance in food-related tapu and noa.**
- Store food in food-only areas. (Do not mix food and non-food items.)
- Use receptacles for food and water for eating and drinking purposes only.
- Do not pass food over the head of kaumātua.
- Keep food surfaces (tables, benchtops) exclusively for purposes related to food.
- Do not put bedding, clothing, toiletries, hairbrush, flannels or urinals on food tables.
- Do not put food on beds, chairs or other non-food surfaces.
- Do not sit on tables, benchtops or surfaces used for food or medication.
**Tapu and noa are key concepts that apply to many areas of life, not just to eating and drinking.
Mātauranga Māori
As well as observing tikanga (above), you can promote mātauranga Māori (Māori knowledge) around kai and wā kai (mealtimes) by inviting or offering a blessing of kai with karakia (prayer) before eating. Creating opportunities to share kai with whānau/family and offering kai Māori (traditional foods) are other ways to support mātauranga Māori.
Example of a blessing for food***
Listen to audio of this karakia
***This just one example of a karakia. Check with kaumātua about their preferred karakia.
| Te reo Māori (Māori language) | English |
|
Whakapaingia ēnei kai Hei oranga mō a mātou tinana Me ō mātou wairua hoki Āmene |
Bless this food To nourish our bodies And our spirits Amen |
Troubleshooting
If you notice that the kaumātua has a change in their relationship with kai (they are not eating or drinking), the reason may be either acute ill health or a tikanga breach (eg, the kaumātua may not consider ‘breakfast in bed’ a treat if the tray is placed on the bed).
Tapu, noa and mana
Upholding the mana of kaumātua includes observing tapu and noa (as above) as well as supporting them to maintain as much independence as possible with eating and drinking. For example, use light-weight but normal-looking cups and glasses before resorting to adaptive equipment, and use clothes protectors on the lap or tucked in the collar like a napkin.
For further information on any of the above concepts, refer to the Guide for health professionals caring for kaumātua | Kupu arataki mō te manaaki kaumātua.
Assessment
It is recommended that registered nurses in ARC remain alert to the possibility of dehydration in the people living in their care facility (Bunn and Hooper 2019). Dehydration is often associated with low fluid intake, particularly when someone is ill. Medication changes, environmental issues such as high environmental temperatures (summer or heatwave) and proximity of fans, heating and air-conditioning units all impact on hydration status.
Hydration assessment
- Water intake predicts hydration status. However, there is no globally accepted evidence on which to base a recommended daily dose (volume) of water for frail older people living either at home or in ARC (Hart et al 2020; Masot et al 2020).
- The European Society for Clinical Nutrition and Metabolism (ESPEN) and the European Food Safety Authority (EFSA) hydration guidelines are the most widely accepted, and they make age-related recommendations. They recommend a daily (24-hour) fluid intake of 1.6 litres for women and 2 litres for men (Masot et al 2020).
- Gaspar (2011) provides a nomogram to tailor fluid levels based on height and weight (see here). According to this scale, those over 75 years of age who are of average height and weight should drink 1.7 litres if female and 1.9 litres if male a day (assuming no contraindications such as a medically initiated fluid restriction). This is similar to the ESPEN and EFSA recommendations.
- Evidence indicates that drinking less than the recommended level, particularly 1 litre or less per day, worsens the effect of chronic conditions (Botigué et al 2019).
- Some evidence indicates that having a low fluid intake (< 1 litre) in a day despite help from care staff is a marker of acute deterioration and impending end of life (Kawakami and Hamano 2020).
- Observable signs of dehydration can be unreliable markers of hydration status. Such signs include dry mouth and tongue, skin turgor, capillary refill time > 3 seconds and concentrated urine (Bunn and Hooper 2019).
- Dehydration can cause acute confusion, change in speech and memory and acute fatigue and hypotension (Hart et al 2020). Dehydration also contributes to constipation.
Nutritional assessment
It is recommended that you assess nutritional status using a standardised tool.
-
The Mini Nutritional Assessment – Short Form is relatively quick to administer and is freely available from the developer from www.mna-elderly.com. It was developed specifically for use in older people and has been used in practice and research for over 25 years (Guigoz and Vellas 2021).
- A nutritional assessment is also included in the interRAI Long-Term Care Facilities assessment.
Hydration population approach
Older people often have a reduced thirst sensation, so it is recommended to set a routine for encouraging fluid intake. Some examples are:
- happy hour with ‘mocktails’
- scheduling regular rounds that offer tea, coffee and other hot drinks (considering mug size and weight)
- social drinking (non-alcoholic) – such as making sharing a drink part of whānau/family visits
- including water bottle holders on walking frames and wheelchairs so drinks are always to hand (plus encouraging participation through diversional therapy to ‘make your own water bottle cover’)
- conducting an internal audit of drinks in reach
- a hydration staff champion
- disguised drinking (ice blocks, jelly, fruit with high water content)
- for warm and hot days, having additional rounds of ‘special’ drinks (eg, iced diet lemonade).
Hydration individual approach
At times, older people living in ARC do become dehydrated. If someone does, it is important to consult with a general practitioner (GP) or nurse practitioner (NP) because the person may need treatment such as subcutaneous or intravenous fluids alongside oral rehydration.
- Studies report subcutaneous fluids are effective for mild to moderate dehydration with minimal complications (Broadhurst et al 2020; Caccialanza et al 2018). A dextrose/ saline solution is recommended, with a GP or NP prescribing a volume of up to 2 litres over 24 hours (Woodward 2013).
- Intravenous fluids are generally restricted to acute hospital care.
Nutritional supplements and diet modification
- A food-first approach is recommended to improve nutritional status. This includes monitoring food intake closely, increasing calorie-dense foods and increasing the frequency of snacks. However, if an older person loses more than 5 percent of their body weight in 3 to 6 months, or 10 percent in 1 month, they are likely to need a referral to a dietitian for further assessment and diet modification, along with a GP or NP review.
- People with swallowing difficulties are likely to need diet modification. The international Dysphagia Diet Standardisation Initiative is the best resource to access for describing modified diets (iddsi.org).
Note: Be aware of the concepts of tapu and noa so you don’t inadvertently discourage hydration. As a result of any breach of tapu, the person may not want to drink.
Care planning
Hydration
- Develop an individual strategy to maintain hydration. Consider setting a fluid goal (within any fluid restrictions). Consider the impact of physical activity, cognition and personal preferences.
- Combine drinking with a fun activity, such as ‘high tea’, ‘happy hour’ and whānau/ family visits (Hart et al 2020).
- Use fluid intake charts only when clinically indicated.
Nutritional
- The Mini Nutritional Assessment provides a treatment guide for assessed level of need.
Māori culture
- Identify surfaces for food, oral medication and inhaled medications only (observe tapu and noa principles). Topical medications should not share the same surface as food.
- Ask what the kaumātua prefers for blessing of food before eating (and who will provide it).
- Find out their preferred place to eat (eg, dining room or sitting in chair rather than ‘breakfast in bed’).
- Ask about their food and drink preferences when they are sick (as it’s important to stay well-nourished and hydrated during this time).
Other cultural preferences
- Ask about traditions, preferences and protocols. Many cultures have food-specific practices.
Nomogram
Recommended water intake in ARC (Gaspar 2011)
- To use the nomogram, find the person’s height (left scale) and weight (right scale) draw a line joining the two points, then read the recommended fluid intake off the centre scale.
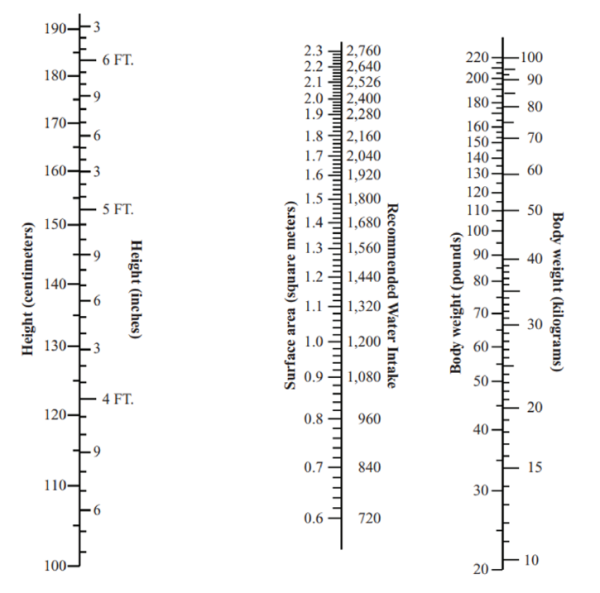
Source: Gaspar 2011
View a higher resolution version of this image in the relevant guide.
Decision support
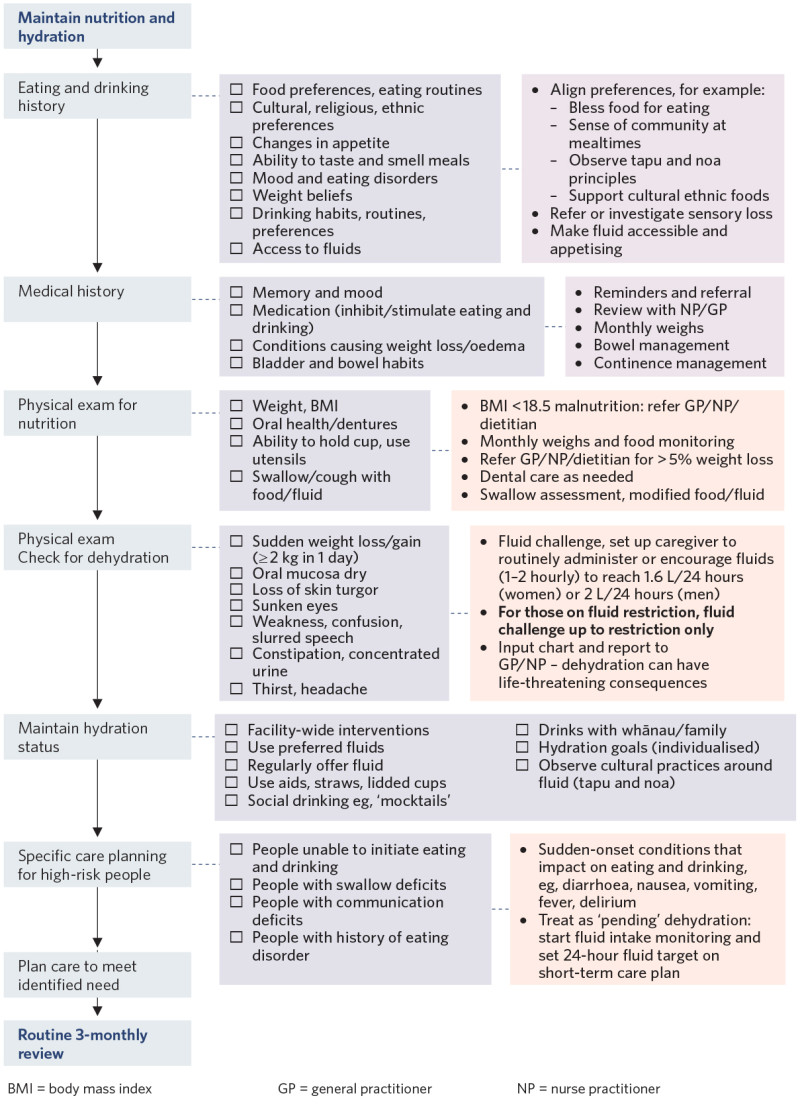
View a higher resolution version of this image in the relevant guide.
References | Ngā tohutoro
Botigué T, Masot O, Miranda J, et al. 2019. Prevalence and risk factors associated with low fluid intake in institutionalized older residents. Journal of the American Medical Directors Association 20(3): 317–22. DOI: 10.1016/j.jamda.2018.08.011.
Broadhurst D, Cooke M, Sriram D, et al. 2020. Subcutaneous hydration and medications infusions (effectiveness, safety, acceptability): a systematic review of systematic reviews. PLoS ONE 15(8): e0237572. DOI: 10.1371/journal.pone.0237572.
Bunn DK, Hooper L. 2019. Signs and symptoms of low-intake dehydration do not work in older care home residents: DRIE Diagnostic Accuracy Study. Journal of the American Medical Directors Association 20(8): 963–70. DOI: 10.1016/j.jamda.2019.01.122.
Caccialanza R, Constans T, Cotogni P, et al. 2018. Subcutaneous infusion of fluids for hydration or nutrition: a review. Journal of Parenteral and Enteral Nutrition 42(2): 296–307. DOI: 10.1177/0148607116676593.
Gaspar PM. 2011. Comparison of four standards for determining adequate water intake of nursing home residents. Research and Theory for Nursing Practice 25(1): 11–22.
Guigoz Y, Vellas B. 2021. Nutritional assessment in older adults: MNA® 25 years of a screening tool and a reference standard for care and research; what next? The Journal of Nutrition, Health & Aging 25(4), 528–83. DOI: 10.1007/s12603-021-1601-y.
Hart K, Marsden R, Paxman J. 2020. Generation of thirst: a critical review of dehydration among older adults living in residential care. Nursing and Residential Care 22(12): 1–12. DOI: 10.12968/nrec.2020.22.12.6.
Hooper L, Bunn DK, Downing A, et al. 2016. Which frail older people are dehydrated? The UK DRIE study. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 71(10): 1341–7. DOI: 10.1093/gerona/glv205.
Kawakami Y, Hamano J. 2020. Changes in body mass index, energy intake, and fluid intake over 60 months premortem as prognostic factors in frail elderly: a post-death longitudinal study. International Journal of Environmental Research and Public Health 17(6): 1823. DOI: 10.3390/ijerph17061823.
Lukito W. 2021. Current evidence in water and hydration science. Annals of Nutrition & Metabolism 77 (Suppl 4): 1–6. DOI: 10.1159/000521769.
Masot O, Miranda J, Santamaría AL, et al. 2020. Fluid intake recommendation considering the physiological adaptations of adults over 65 years: a critical review. Nutrients 12(11): 3383. DOI: 10.3390/nu12113383.
Mead HM. 2016. Tikanga Māori: Living by Māori values. Wellington: Huia.
Popkin BM, D’Anci KE, Rosenberg IH. 2010. Water, hydration, and health. Nutrition Reviews 68(8): 439–58. DOI: 10.1111/j.1753-4887.2010.00304.x.
Woodward M. 2013. Guidelines to Effective Hydration in Aged Care Facilities. URL: www.mcgill.ca/familymed/files/familymed/effective_hydration_in_elderly.pdf.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
