To return to the list of all of the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
Contents
- Definition
- Why this is important
- Implications for kaumātua
- Assessment
- Treatment
- Care planning
- Decision support
- References | Ngā tohutoro
The information in this guide is accurate to the best of our knowledge as of June 2023.
Definition
Constipation describes a set of difficulties associated with defecation that a person experiences more than a quarter of the time. These difficulties include hard, lumpy, difficult-to-pass stools, straining, the feeling of incomplete emptying, infrequent bowel opening (fewer than three times a week without laxatives) and the need to manually assist defecation. Constipation may be acute (lasting less than 1 week) or chronic (lasting for 3 months or more). The need for regular aperients (laxatives) is diagnostic for underlying constipation (Aziz et al 2020).
Key points
- Constipation occurs in up to half of all people living in aged residential care (De Giorgio et al 2015; Mounsey et al 2015).
- Chronic constipation is best managed with a long-term plan and ongoing review.
Why this is important
Constipation has a significant impact on quality of life. While nurses in aged residential care commonly manage the problem, it can also progress to a bowel obstruction – a life-threatening condition.
Implications for kaumātua*
Some kaumātua may experience a sense of whakamā (shame, embarrassment) about their constipation and therefore not disclose their difficulty in passing stools. One reason for this may be that the kaumātua is a private person so finds it difficult to discuss such topics.
See the Guide for health professionals caring for kaumātua | Kupu arataki mō te manaaki kaumātua for more information.
It is essential to give kaumātua and whānau/family all the information they need to fully participate and engage in preventive interventions and treatment. This might include explaining the importance of physical exercise, fibre-rich food and adequate hydration, and supporting appealing options that align with cultural preferences (eg, kapa haka to keep active, consuming kiwifruit products or traditional Māori herbal remedies).
Using familiar, culturally acceptable terms when discussing constipation and bowel habit may help the kaumātua to communicate more freely.
Kupu (words) to discuss constipation
| Māori term and pronunciation | English translation |
| Tūtae, hamuti | Stool, faeces |
| Tiko | Defecate |
| Turuturu | Leak |
| Kope | Pad |
| Wharepaku | Toilet |
| Uaua | Difficult |
| Mārō | Hard |
| Ngohengohe | Soft, pliable |
*Kaumātua are individuals, and their connection with culture varies. This guide provides a starting point for a conversation about some key cultural concepts with kaumātua and their whānau/family. It is not an exhaustive list; nor does it apply to every person who identifies as Māori. It remains important to avoid assuming all concepts apply to everyone and to allow care to be person and whānau/family led.
Assessment
The caregiver is often the one who identifies constipation. It is the nurse’s responsibility to respond to that report using a diagnostic reasoning process: taking the history, conducting a physical examination and often treating with prescribed ‘as needed’ (PRN) medication. As part of this process, it is important to:
- assess bowel habit with the Bristol stool chart
- distinguish between constipation and bowel obstruction (potentially life threatening) and recognise any need for referral
- consider likely causes of constipation
- have a good knowledge of the different laxatives available (see table in ‘Laxatives’ section) to administer PRN treatment successfully.
Treatment
Constipation: population approach
1. Avoid constipation (Aziz et al 2020).
a. Provide fluid rounds to encourage intake.
b. Provide additional fluid support on hot days.
c. Build regular physical activity into facility routines.
d. Undertake routine dietary review of facility menu for fibre and stimulant content.
Constipation: individual approach
1. Avoid constipation.
a. Assess and address key causes of constipation.
b. Consider appropriate laxative management.
c. Discuss laxative management with prescriber: regular laxatives may be required.
d. Monitor bowel function to titrate laxative.
2. Treat acute constipation.
a. Assess and address key causes of constipation: consider recent changes.
b. Consider appropriate laxative selection from PRN medication.
c. Escalate to general practitioner (GP) or nurse practitioner (NP) if acute constipation is not resolved in 3 days.
d. Monitor bowel function to titrate laxative.
3. Be aware of risk of bowel obstruction. Severe constipation can evolve into a bowel obstruction, which is a clinical emergency that requires urgent assessment.
a. A cognitively impaired resident may not report or may not be able to report bowel function. If their behaviours change, investigate for constipation.
b. Where a resident has episodes of loose bowel motions, assess for severe constipation with overflow.
c. When assessing nausea, vomiting or abdominal pain, always investigate bowel function as well.
Care planning
In the care plan, include:
- fluid intake, adjusted during warm weather
- physical activity as tolerated (including incidental walking, eg, to toilet)
- individual dietary supplements (eg, dried fruit, grapes)
- selection of fibre-rich food from standard menu (eg, porridge rather than toast for breakfast)
- regular and PRN laxatives.
Bristol stool chart
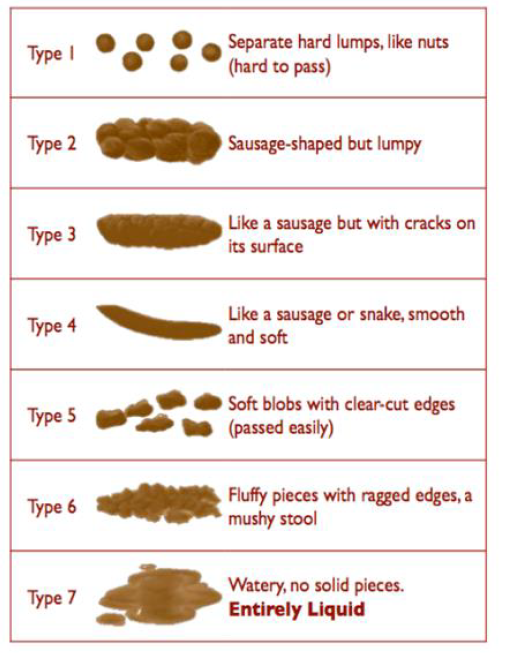
Source: http://www.continence.org.au/bristol-stool-chart
View a higher resolution version of this image in the relevant guide.
Laxatives
Do not give laxative if you suspect a bowel obstruction
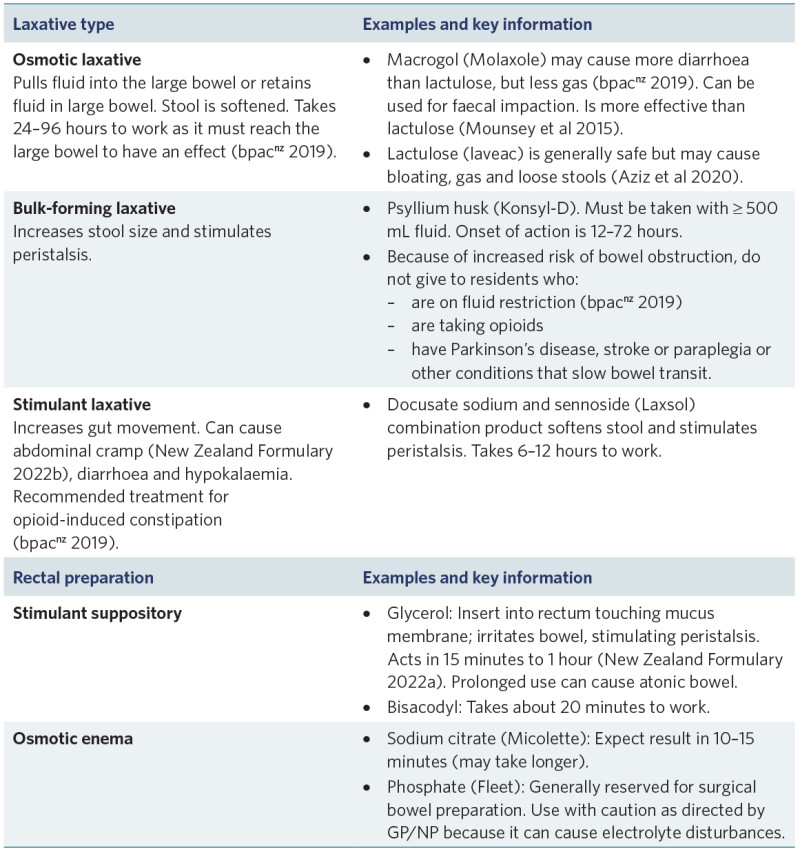
View a higher resolution version of this image in the relevant guide.
Decision support
Bowel management to avoid constipation
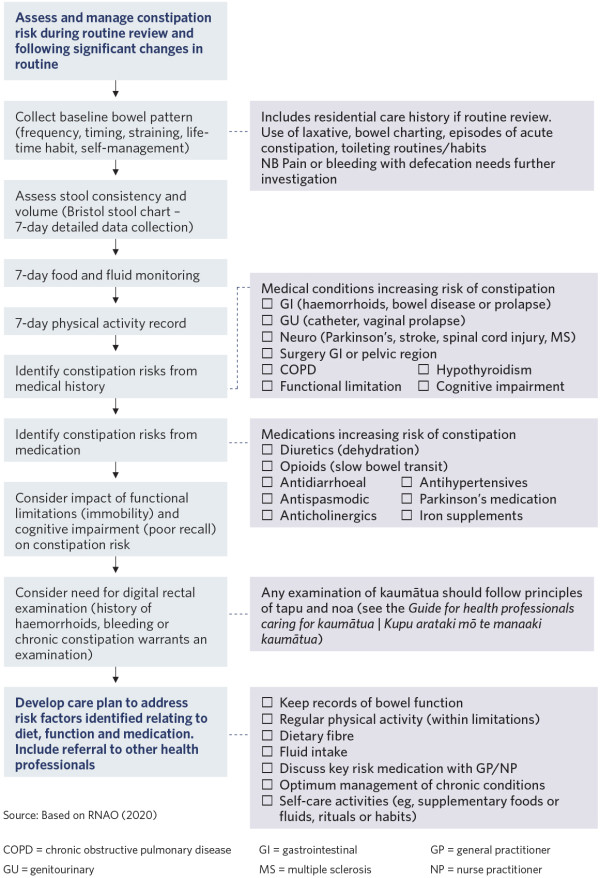
View a higher resolution version of this image in the relevant guide.
Responding to acute constipation
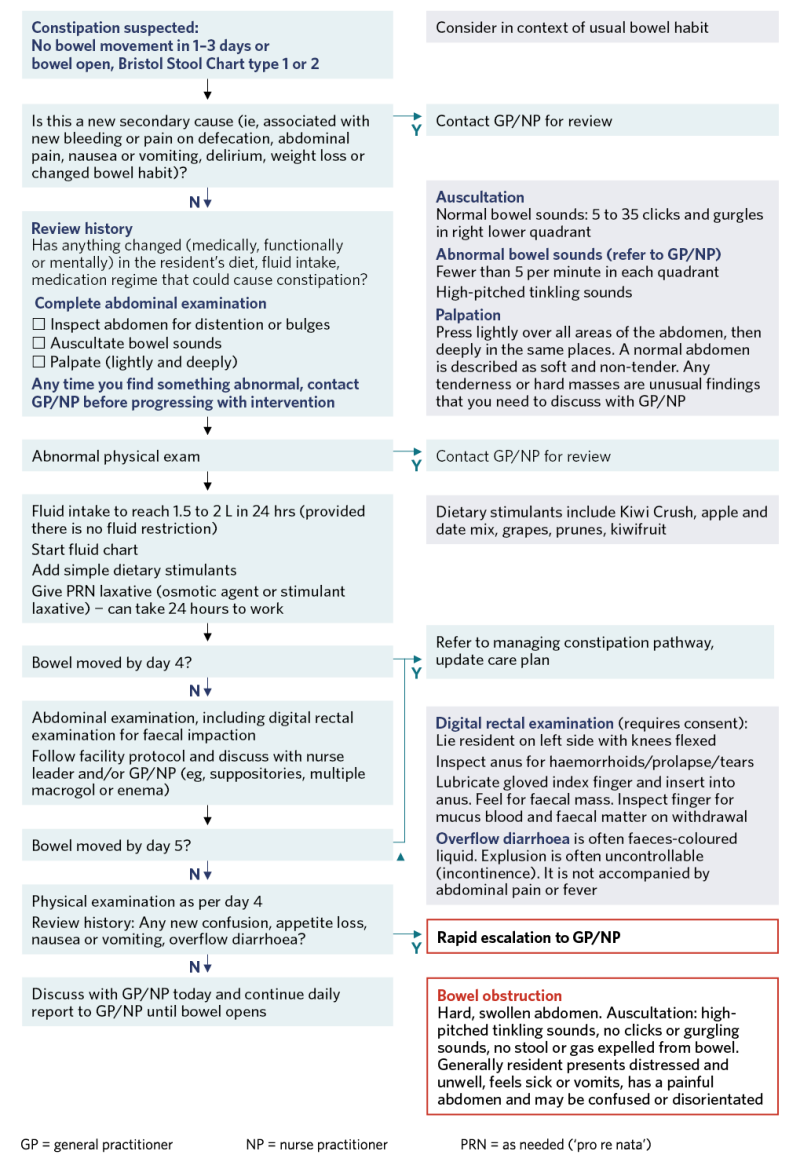
View a higher resolution version of this image in the relevant guide.
References | Ngā tohutoro
Aziz I, Whitehead WE, Palsson OS, et al. 2020. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Review of Gastroenterology & Hepatology 14(1): 39–46. DOI: 10.1080/17474124.2020.1708718.
bpacnz. 2019. Managing Constipation in Older People. Dunedin: Best Practice Advocacy Centre New Zealand. URL: bpac.org.nz/2019/docs/constipation.pdf.
De Giorgio R, Ruggeri E, Stanghellini V, et al. 2015. Chronic constipation in the elderly: a primer for the gastroenterologist. BMC Gastroenterology 15: 130. DOI: 10.1186/s12876-015-0366-3.
Mounsey A, Raleigh M, Wilson A. 2015. Management of constipation in older adults. American Family Physician 92(6): 500–4.
New Zealand Formulary. 2022a. Glycerol (rectal). URL: nzf.org.nz/nzf_878.
New Zealand Formulary. 2022b. Laxatives. URL: nzf.org.nz/nzf_852.
RNAO. 2020. A Proactive Approach to Bladder and Bowel Management in Adults (4th edn). Toronto: Registered Nurses’ Association of Ontario. URL: rnao.ca/sites/rnao-ca/files/bpg/Bladder_and_Bowel_Management_FINAL_WEB.pdf.
If you have feedback about the Frailty care guides | Ngā aratohu maimoa hauwarea, click here.
